Introduction to Pressure Injury.
The human body isn’t built for prolonged immobility, and patients in healthcare settings face the risk of pressure injuries, formerly known as bedsores or decubitus ulcers. This article delves into the causes, stages, and legal aspects surrounding pressure injuries.

Prevalence and Regulation
Healthcare facilities, particularly nursing homes, often encounter pressure injuries or bedsores, leading to claims and legal implications. State and federal regulations emphasize prevention and treatment, acknowledging negligence in nursing care as a common cause.
How does pressure injury or bedsores occur?
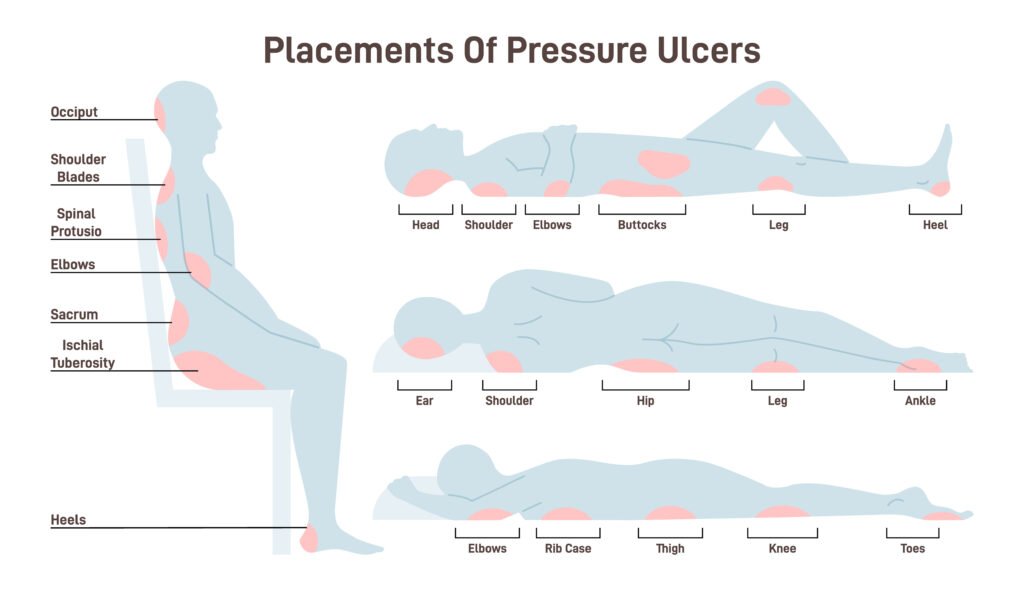
Prolonged pressure, primarily on bony prominences, can result in pressure injuries. Factors such as duration, pressure intensity, skin health, and shear or friction contribute to the severity. Patients with thin build, poor blood perfusion, or incontinence face higher risks.
Stages of Bedsores
Pressure injuries are staged based on severity.
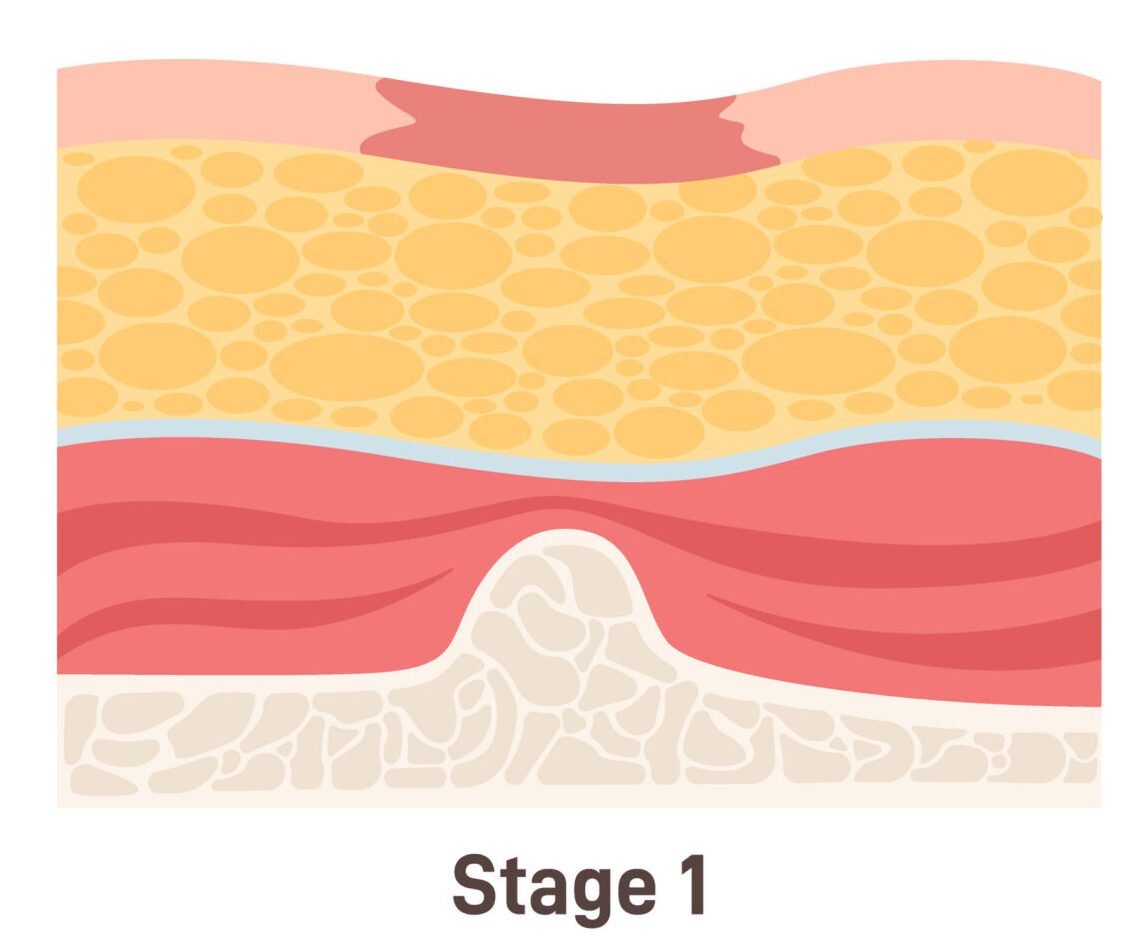
Stage I Pressure Injury
The skin turns red and doesn’t go back to its normal color when pressed, signaling the start of an issue.
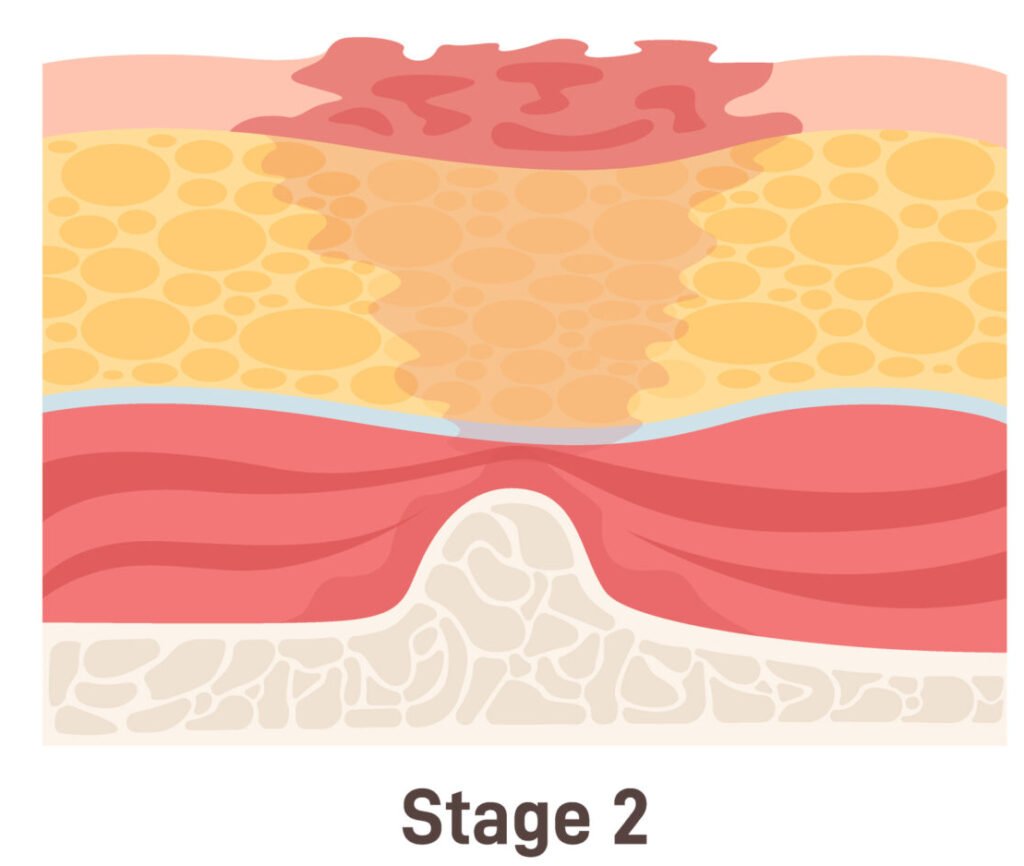
Stage II Pressure Injury.
The skin gets a blister or tear, showing damage not just on the surface but also underneath.
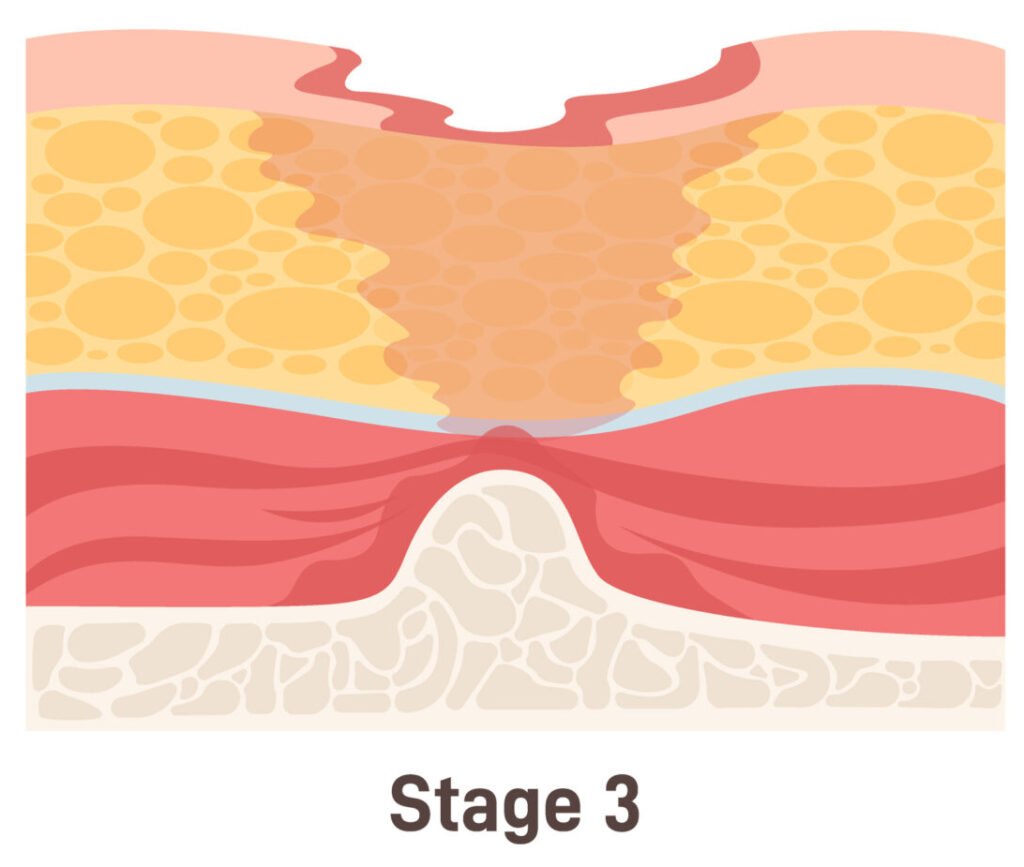
Stage III Pressure Injury.
The injury goes deeper into the skin, requiring special care and attention to prevent it from getting worse.

Stage IV Pressure Injury.
The damage reaches the bone, becoming a serious problem with a risk of infection, needing intense treatment, and possibly leaving a lasting injury.
Meeting the Standard of Care: Prevention
Prevention involves the nursing process: assessment, planning, intervention, and documentation. The Braden Scale helps assess risk factors, guiding the care plan. Regular skin assessments and consultations with wound specialists are crucial.
Meeting the Standard of Care: Treatment
CMS guidelines dictate interventions, emphasizing pressure relief or “offloading” through repositioning every two hours. Specialized mattresses or beds may be recommended based on the patient’s condition.

Proving Fault in a Lawsuit
Wound photos serve as crucial evidence in pressure injury cases, showcasing negligence and the pain involved. Proving causation, particularly in sepsis-related deaths, requires a thorough analysis of medical records and expert testimony.

Finding Fault in the Medical Record
Examining records involves scrutinizing repositioning schedules, positions, and the adequacy of care plans. A root cause analysis identifies negligence, often tied to understaffing issues.
What the facility will claim
Defense strategies often involve claiming unavoidable pressure injuries due to comorbidities or patient refusal. Plaintiffs counter by by proving interventions were not implemented.
Conclusion
Pressure injury cases vary, considering neglect severity, injury extent, and the forum. Evidence of understaffing, disregard, and facility issues can influence jury decisions, emphasizing the need for diligence in preventing pressure injuries.